
Podcast: Play in new window | Download (Duration: 39:55 — 32.8MB) | Embed
Subscribe: Apple Podcasts | Spotify | Email | RSS | More
Dr. Motley studies emerging black males & females with mental illness compounded by racism & violence. They need support systems & a chance for upward mobility.
About the Show
Welcome to Health Hats, learning on the journey toward best health. I am Danny van Leeuwen, a two-legged, old, cisgender, white man with privilege, living in a food oasis, who can afford many hats and knows a little about a lot of healthcare and a lot about very little. Most people wear hats one at a time, but I wear them all at once. I’m the Rosetta Stone of Healthcare. We will listen and learn about what it takes to adjust to life’s realities in the awesome circus of healthcare. Let’s make some sense of all this.
We respect Listeners, Watchers, and Readers. Show Notes at the end.
Watch on YouTube
Read Newsletter
The same content as the podcast, but not a verbatim transcript. Could be a book chapter with images. download the printable transcript here
Contents
Exposure to community violence 03:54. 2
Emerging and experiencing violence and mental illness 06:12. 3
Breaking the cycle – support systems 08:05. 3
Breaking the cycle – transportation 08:44. 3
Breaking the cycle – belonging 10:51. 4
Breaking the cycle – upward social mobility. 4
A word from our sponsor, Abridge 11:40. 4
Identifying the research question 13:54. 5
Staying in touch, up to date 16:06. 5
Think, read, write, talk 18:10. 6
Measuring police violence 18:49. 6
Vacuum-filler, gap filler 20:55. 6
Community Advisory Board 23:00. 7
People with lived experience analyzing study results 25:31. 7
Research without implementation – ink on paper 26:22. 8
Community uptake of research 29:49. 8
Episode
Proem
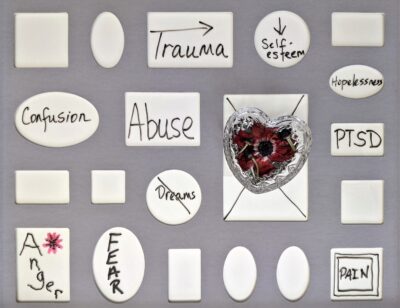
Image by Susan Wilkenson on Unsplash
Trauma and mental illness seem inexorably linked with racism and homelessness contributing to severity and complexity. How do we know? Does evidence exist? Do we even need proof? Isn’t it obvious? I think I need to speak with a social worker, researcher. Fortunately, I met Whitney Irie, Ph.D., MSW, Assistant Professor at Boston College School of Social Work, who introduced me to Robert Motley, Ph.D., MSW, also at Boston College. Robert examines the intersection of racism, violence, and trauma for emerging black adult men and women ages 18-29 and associated mental and behavioral outcomes. Eureka, a match!

Image by Stefano Pollio on Unsplash
Podcast intro
Welcome to Health Hats, the Podcast. I’m Danny van Leeuwen, a two-legged cisgender old white man of privilege who knows a little bit about a lot of healthcare and a lot about very little. We will listen and learn about what it takes to adjust to life’s realities in the awesome circus of healthcare. Let’s make some sense of all of this.
Exposure to community violence
Robert Motley: During my doctoral studies, my research focused on exposure to community violence among black emerging adults. I conducted a systematic literature review on trauma. What was the prevalence of trauma among black males? What were some barriers or facilitators to using mental health services? Looking at the literature, we found high levels of trauma exposure for black men: 50% to 60% had experienced trauma, some of them seven or eight times during their lifetime. They also had high rates of mental health illnesses such as anxiety, generalized anxiety, psychotic disorders, etc. But the most critical finding was that roughly 56% to 74% of the black males across these studies may have had an unmet need for mental health services.
So, you’re talking about a large population of black men walking around what I like to call ticking time bombs because they are experiencing a lot of traumas. And we know the adverse effects of trauma on one’s mental health. But when you’re not receiving services, it could intensify many of the symptoms they’re already exhibiting or experiencing.
Emerging adults
Health Hats: Wow. When I spoke to you earlier, it was the first time I heard the phrase emerging adults. I love it. I love it so much that I changed the series title from Young Adults with Mental Illness to Emerging Adults with Mental Illness. Emerging feels much more powerful. How did this term evolve?
Robert Motley: I didn’t know this term until 2015 myself. I was at a conference with a workshop called Emerging Adulthood. Dr. Jeffrey Arnett coined the phrase. Advances in technology can prolong the transition into adulthood. They take more time before they take on the responsibilities of adulthood: meaning that you marry, have children, enter your career, and you’re no longer depending on your parents for any type of financial support. Because people stay in school longer, they’re still in this transitional period where they’re trying to figure out what they want to be and what type of career they want. They’re still exploring love possibilities and things like that. So that period between 18 to 29 years old is what Jeffrey Arnett coins as emerging adulthood. Some focus more on 18 to 25, but it extends up to 29.
Emerging and experiencing violence and mental illness
Health Hats: Emerging adults that experience severe mental illness plus racism, homophobia, and sexism have an even more diminished chance of finding treatment and support. This is so complex. The likelihood of community violence and incarceration is also increasing. There are so many forces here. How can that be broken? It freaks me out. It’s not just starting on a back foot. It sounds like with your butt in the air.
Robert Motley: It just keeps going. How do you stop the Ferris Wheel from continuing? It just keeps going. How do people get off to get the help they need for emerging adulthood? A lot can be done, but I don’t want to discuss emerging adults as a whole group. We must be specific with the population we’re talking about and the problem. I will speak to that population since I research black emerging adults.
Health Hats: Do you speak to black males or also black females?
Robert Motley: Most of the work that I do now encompasses both black males and black female emerging adults.
Breaking the cycle – support systems
Robert Motley: When we think about how we break this cycle, there are a couple of ways. From some of the research I’ve been doing, we have found that having some type of support system that you can lean on is very important because, without any support, you’re stuck dealing with these things on your own. And when you’re experiencing these symptoms, a lot of times, it’s just hard to try to manage it on your own. So having a support system is essential.
Breaking the cycle – transportation
We also found that people with mental illnesses have some transportation services to take them from where they are to the needed care, wherever that facility may be. That is a big thing that has come out in the research, particularly in focus groups with emerging adults suffering from mental illness.
Breaking the cycle – belonging
I interned at a drop-in center at a facility that served individuals living with a severe mental illness, almost their home away from home. The drop-in center is where they can be around people who are like them and who they get along with.
But they had clinicians on staff that could work with them. They had game rooms. They had different groups about how to live better and navigate the hospital systems. How do you get connected with mental health providers? They had so much support at these drop-in centers. I feel that having more of these drop-in centers and areas with high rates of mental illnesses will be another way we can break this cycle because they need help. We need relentless and sustained engagement with this population to facilitate better access to the required services. It can’t be a one-off. You must have services in place that are going to be sustained and long-term that can be in place to be able to assist these individuals with getting the different services that they need. Because for a lot of them, transportation, they don’t have any money. They may be secluded; they don’t have a lot of friends. What can we put in place to have individuals who can go out into the communities and assist them, taking them to a clinician or a mental health facility to get the services they need?
Breaking the cycle – upward social mobility
Lastly, they need more opportunities to allow these individuals upward social mobility. What do I mean by upward social mobility? I identify three key factors: education, employment, and income. Could they advance their education, get the skills needed to get a good job, be livable, and earn livable wages?
When you have individuals with no upward social mobility, they’re often stuck in areas with low income, poverty, crime, etc. So, they’re more susceptible to continuing the cycle. Being exposed to violence, not knowing where to get the services, not having any support. It must be a relentless and tailored intervention approach for this population if we want to genuinely break the cycle for them.
A word from our sponsor, Abridge
Now a word about our sponsor, ABridge. Record your healthcare conversations with doctors and other clinicians with ABridge. Push the big pink button and record. Read the transcript or listen to clips when you get home. Check out the app at ABridge.com or download it from the Apple app store or Google Play store. Let me know how it went.
Call to action
I need help. I’ve expanded my podcast this year to include video, and costs have surged to $15,000 annually, while each episode takes 30 to 40 hours to produce. With growing content and shrinking bandwidth, I need support to keep creating without impacting our retirement funds.
As I look towards the next 5-10 years, I’m building a production team of emerging adults to carry this project forward. This succession planning requires resources. But here’s the deal: you can help.
Visit health-hats.com/support for ways to contribute. Best option? Patreon offers a monthly subscription with bonus content, Zoom meetings with me and fellow contributors, personal Bari Sax MP3s, coaching sessions, and more.
Occasional donations are welcome, and you can still subscribe for free to enjoy bonus episodes. You can also recommend us through email, social media, or postcard – postage on us! Visit health-hats.com/support. Your support is deeply appreciated. Thank you.
Identifying the research question
Health Hats: Wow. So, you’re a researcher. How do you identify the research questions you invest your time and energy in? You’re not a newbie researcher anymore. You’re a mature researcher. How do you know that you’re asking the right questions?
Robert Motley: Yeah. Great question. The great thing about my job is that you pick a research area or topic that is most important to you. So being a black man growing up on the west side of Chicago, knowing what I’ve experienced, I was interested in community violence. I wanted to study black populations, black emerging adults. As a researcher, when starting, you must first find out what has already been done. The big task is to do a scoping review of the different types of research. I would go back 20 years to say what researchers have been doing on topics around community violence exposure for black emerging adults looking at mental health outcomes, behavioral health outcomes, etc.
Gaps in research
I wanted to know what has been done, what has been tried, what research questions have been proposed, and that I would be able to identify what hasn’t been asked based on the research that has been done. Any researcher out there looking at a topic, you want first to find out what has already been done around this topic. Cause we’re trying to identify research gaps that we can then fill. These gaps affect future research questions, practice, and policy implications. And so that was the way that I came up with my questions regarding my research projects.
Staying in touch, up to date
Health Hats: Now that you are more mature at this and you have a lab, if you’re anything like me, you are at risk of being at full yourself. Let me just give you an example. Recently I had as a guest a young lady in her mid-twenties who’s very much working with young adults with complex and rare medical conditions. And she’s apprehensive about being out of touch with 13-year-olds at 25, and I just loved about her that that was her concern. It seems like when it comes to racism and community and violence, not that this is my field of expertise, but there seem to be certain core things you probably don’t need to research to know they’re there. Yes. But then there’s stuff that every era has a new twist. When I was young, meaning just 20 years ago, even ten years ago, social media wasn’t as big as it is. How do you ensure you stay in touch with the new stresses contributing to community violence?
Think, read, write, talk
Robert Motley: Great question. I always tell people when they ask what I get paid to do as a researcher. We get paid to think, read, write, and talk. Once you stop doing those things, you will no longer have a job. And so, the only way that I could keep abreast of the changes happening within society and for the populations that I’m most interested in is to stay on top of the research that is being published. I must stay engaged and not only in the work. How am I conceptualizing the problems that are happening to this population?
Measuring police violence
Back in 2014, when police violence started kicking up after the killing of Michael Brown in St. Louis, where I was living, you saw many researchers investigating police violence and its impact on black populations. When Michael Brown was killed in Ferguson, Missouri, you started to see the influx of research papers and op-eds talking about police violence and the prevalence of race. And since then, you’ve had many articles come out, right? But one of the things that I looked at was that being exposed to police violence is just one thing. All of us, no matter what color we are, can be exposed to police saying something derogatory towards us or grabbing us when we feel like they shouldn’t have held us and things like that. I was most interested in how we examine the frequency of people exposed to police violence, that they perceive that the actions of the police are because of the color of their skin. Okay. And that’s what I call perceived racism-based police violence. How do we measure it to be able to capture those experiences? When I looked at the measures on racism and things like that, no existing measure would allow me to capture the frequency of their exposure. Not just as a witness but also when you see videos in the media that you perceive as racism-based police violence. So, I had to develop a measure for that, which I did. That was me adding value to science by creating a measure now that other researchers can use to assess the frequency of exposure to perceived racism-based police violence. That’s one of the things that when you’re keeping up with what’s going on, we’re thinking about our population and where’s the gap, where people are not thinking about? That was one of the ways that I could come up with a new area of research that was not just looking at community violence exposure, but a specific type of community-based violence exposure.
Vacuum-filler, gap filler
Health Hats: That’s interesting. During my career in nursing and then in administration, quality management, and information technology, I thought of myself as a vacuum filler, which is similar. Where are the gaps, and fill them? I find that to be very fascinating. Why is something a gap? Why is there a gap in care? Why is there a gap in understanding? Why is there a gap in measurement? Why is there a gap in action? And it seems like those are the places where there’s plenty of expertise around them, but it’s not being applied, and then to be able to build a bridge or a method, or a threshold, or something, I find that to be exciting work. But wait a minute, how do you find gaps you don’t see yourself?
During our brief introductory call, we discussed how you include emerging adults with lived experience in your research design, analysis, and dissemination. Can you talk a little bit about that? How does that help you feel authentic, up-to-date, genuine, and on track?
Community Advisory Board
Robert Motley: I love to conduct mixed methods research where we collect qualitative and quantitative data. I say focus groups or individual interviews with black emerging adults when discussing qualitative data. So that gives me in-depth insight into their lived experiences, expertise, and deeper perspective of what’s happening to them. How are they perceiving what’s going on with them? What do they feel they need to overcome some of the obstacles they face? With that rich data, we have a more thorough understanding of what is going on with the population. But then also how do I get them engaged in my, so that’s one way. Another way is a project that I’m working on now, where I created a community advisory board which is a community advisory board of emerging adults. And so, I have a grant from Robert Woods Johnson Foundation where I’m looking to validate the measure I developed for my dissertation. Still, now with the national sample of black emerging adults and Latinx emerging adults or Hispanic, they’re different terms, but we use Latinx.
The Community Advisory Board consists of black and Latinx emerging adults speaking English and Spanish, and they are involved in helping me to create and adapt survey items that can precisely capture their experiences. These are people from the population I have been involved in, allowing me to think through and develop the best survey items. And then I will then conduct individual interviews with both Black and Latinx emerging adults to also share the items to get their feedback based on their lived experiences before I pilot to a much larger sample.
Having a community of advisory boards and expert content panels are ways to get people from the population engaged in the research’s development and beginnings before you implement it with a much larger sample. It’s more rigorous. I love that process because they can give you some of their lived experience, look at some of your thoughts, and say, no, this is something that you’re missing where you’re not capturing for this population. It strengthens the research.
People with lived experience analyzing study results
Health Hats: Do you ever seek their assistance to analyze the results? Like to analyze, analyze the results of the studies.
Robert Motley: Yes, right now, once they helped me to come up with the items, we now go, and we do our interviews. Once we came back with that data, they helped to look at, okay, what was some of the, the, the things that the respondent said that they didn’t understand about the questions, so collect collectively as a group. We say, okay, what do we need to take from these responses to modify these survey items a little bit more, refine them, and tune them so that we’re all pleased with the final set of items we have?
Research without implementation – ink on paper
Health Hats: That’s rich. Research without implementation seems to me to be ink on paper. The challenge is that you do good work and identify something that, if generalized in more communities, might help reduce community violence or increase the proportion of emerging adults with serious mental illness who have meaningful lives. Just because something is evidence-based doesn’t mean anybody will adopt it. How does what you learn spread into the diaspora of all these different, emerging entities, black emerging adults, communities beyond Boston or Missouri, or the west side of Chicago? What do you think about that?
Robert Motley: It’s a tall task, and as researchers, we’re always trying to conduct research that has implications for practice and embed these things within organizations. I always look to partner with existing community-based organizations, particularly those that provide some type of prevention or intervention around mental health services. Building those relationships is good because I want to use my findings to immediately impact the population when I develop a research idea. One example is what I’m doing now with my project.
Strategies for Youth
I have an organization here in Cambridge, Massachusetts, called Strategies for Youth. I met Lisa Thurau, executive director when I first got to Boston. They do a lot of training with law enforcement officials nationwide to train them on techniques to better engage the younger black populations. But they hadn’t done anything around emerging adults. When I was speaking with them, I told them I was applying for this grant. They’re committed to saying, okay, Robert, you conduct your research. When you return with the findings, we will take your results to modify the existing training we do with law enforcement. So now it can be inclusive of the experiences of black emerging adults so that now police officers can, can be trained on how to engage properly with this population so that we have fewer negative interactions with police and black emerging adults.
Community uptake of research
That’s one win. Now we must evaluate whether it has its intended impact. And once you do a rigorous evaluation, you see it has its effect. Now how do we scale up to take it national? It’s a lot of steps to get across the country, but when you do it right at the beginning, and you build the foundation then it, it should be a more accessible sale. Because as you say, I believe that all organizations should be using interventions or preventions that have, that are evidence-based. How do you make them aware of these evidence-based practices? I try to work with organizations cause a lot of them have ties to other organizations across the country. And things like that. I’m also working with Dr. Craig Burns, the director of the University Counseling Services at Boston College. Once I develop this measure for this large national sample, we will have an event to invite all mental health professionals working in college, university, or community-based organizations that provide mental health services. We will have an event to talk with them about this scale with the hopes of them including it when assessing trauma for Black and Latinx emerging adults. We’re trying to institutionalize this measure and embed them in these organizations. And so, strategically, I try to work with organizations, not just to do the work research, but how am I implementing it into practice? So those are two.
Health Hats: I love it. I’m on the board of Governors of PCORI (Patient-Centered Research Outcomes Institute). I’m a heavy advocate for community-based research funding with research designed to increase the likelihood of community uptake. I had ideals and energy and didn’t know that much. I’ve realized how difficult it is to apply for research funding. It’s a skill, and you need experience at that, and it isn’t what community organizations do. And it isn’t. It’s not how they should spend their money. That’s your job. You are the researcher. You’re the one who needs to be an expert at where’s the money and, how you get it, and how do you design the study. And so, I try to encourage community organizations to partner with researchers and invest in those partnerships. That’s how community organizations benefit from what they’ve learned by working with the populations they love and support and get information they can leverage to do their work better through partnerships. I love hearing it from your side.
This is great. What haven’t we talked about that we ought to?
Robert Motley: There’s a lot to talk about.
Health Hats: We’re both good talkers. Both of our business is talking.
Social media
Robert Motley: We didn’t talk about social media. You mentioned earlier that social media is such a new phenomenon. Now we’re trying to tease out the effect that social media can have around violence and how exposure to violence via social media can impact the mental health of black emerging adults.
We do have a couple of pieces that have been published and some that are forthcoming that have been looking at the amount of exposure to police violence videos or to police violence that you perceived as being racism based and how it’s been found to be associated with substance use but also suicidality among, among black emerging adults. And now, what do we do about that? Because there is a negative impact from using social media, but there can also be a positive impact because social media has now opened up various pathways. And so let’s just take, for example, a person who may be suffering from mental illness, and they’re in their community, don’t have a support system. Still, if they have access to social media, they have access to friends and family members, not only in their locale but across the country, who they can now connect with. They have opportunities to connect with support groups online with people who have similar lived experiences as them.
They also have telehealth, where you can connect with providers online for needed services. It’s a pros and cons to social media. It depends on how you use it. Those are good things about social media, but it is an impact. It can have a negative effect. This is great, depending on what you’re exposing yourself to when using those platforms. I love talking about my research.
Health Hats: Thank you. Happy holidays.
Reflection
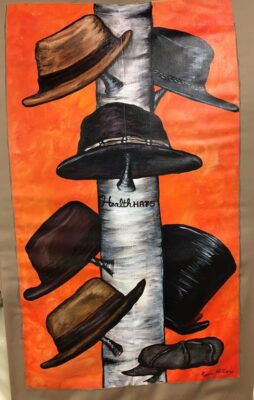
Walking Gallery Jacket by Regina Holliday
Every few years, I re-examine my podcasting/activism purpose and audience. I can confirm that my primary audiences are people who wear some of the hats I wear. You are veterans and emerging experts with lived healthcare experience. You have constituencies of your own. I live to help the helpers. You who serve others are my constituency. To stay current and relevant as local, regional, or national activists, we must continually listen to diverse lived experiences. I’ve blogged, podcasted, and vlogged to learn, muse, and share with you for over ten years. Podcasting and vlogging transform me, and the resulting material can change you by providing a more profound understanding of slices of healthcare and life about which we lack the deep knowledge we crave to keep doing our meaningful work.

This series about people and programs eyeball-deep supporting Emerging Adults with Mental Illness takes a multi-dimensional look into an under-resourced, alienating, frustrating, and inspiring world. In this 12th episode with Dr. Robert Motley, I’ve learned the term emerging adults. In our work and practices, we hear the umbrella of social determinants of health, now a buzzword losing its meaning without more specificity. When Robert discussed breaking the cycle of violence and mental illness, he highlighted support systems, transportation, belonging, and upward social mobility. I can get my teeth into those more than social determinants of health. Robert hooked me on the research gaps, partnering with communities and individuals with lived experience in research and his examples of communities in action. I learned quite a bit. How about you? Has this series expanded your more profound knowledge of the world around emerging adults with mental illness? Let me know.
Podcast Outro
I host, write, edit, engineer, and produce Health Hats, the Podcast. Kayla Nelson provides website and social media consultation and manages dissemination. Joey van Leeuwen supplies musical support, especially for the podcast intro and outro. Leon van Leeuwen edits written material. I play bari sax on some episodes alone or with the Lechuga Fresca Latin Band. I’m grateful to you, who have the most critical roles as listeners, readers, and watchers. See the show notes, previous podcasts, and other resources through my website, www.health-hats.com, and YouTube channel. Please subscribe and contribute. If you like it, share it. See you around the block
Episode Notes
Please comment and ask questions
- at the comment section at the bottom of the show notes
- on LinkedIn
- via email
- YouTube channel
- DM on Instagram, Twitter, Mastadon to @healthhats
Production Team
Web and Social Media Coach, Dissemination Kayla Nelson @lifeoflesion
Leon van Leeuwen edits the article-grade transcript.
Music on intro and outro by permission from Joey van Leeuwen, Drummer, Composer, and Arranger including Moe’s Blues for Proem and Reflection
Other Credits
Images
Vulture Couple by Rich Rieger, used with permission
Woman and Clown by Diana Feil on Unsplash
Trauma post by Susan Wilkenson on Unsplash
Collaboration (Hands on tree) by Shane Rounce on Unsplash
Walking Gallery Jacket by Regina Holliday
Pain (person pressed to glass) by Stefano Pollio on Unsplash
Disclaimer
The views and opinions presented in this podcast and publication are solely my responsibility and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute® (PCORI®), its Board of Governors, or Methodology Committee. Danny van Leeuwen (Health Hats)
Sponsored by Abridge
Inspired by and grateful to Whitney Irie, Amanda Chue, Sneha Dave, Betsy Neptune, Craig Burns, Lisa Thurau, Kristin Carmen, Matt Hudson
Links
Robert Motley, Ph.D., MSW, Assistant Professor at Boston College School of Social Work
Validate the measure developed for dissertation.
Whitney Irie, Ph.D., MSW, Assistant Professor at Boston College School of Social Work
Emerging Adulthood. Dr. Jeffrey Arnett
A new area of research that was not just looking at community violence exposure, but a specific type of community-based violence exposure
Strategies for Youth, Lisa Thurau, Executive Director
Dr. Craig Burns, the director of the University Counseling Services at Boston College
PCORI community-based research
Related podcasts
Series: Pediatric Transition to Adult Care
Creative Commons Licensing
The material found on this website created by me is Open Source and licensed under Creative Commons Attribution. Anyone may use the material (written, audio, or video) freely at no charge. Please cite the source as: ‘From Danny van Leeuwen, Health Hats. (including the link to my website). I welcome edits and improvements. Please let me know. danny@health-hats.com. The material on this site created by others is theirs, and use follows their guidelines.
