Podcast: Play in new window | Download (Duration: 10:01 — 9.8MB) | Embed
Subscribe: Apple Podcasts | Spotify | Email | RSS | More
Why can’t we fill in personal data and routine community COVID stats into a web form and calculate our risk of infection and mortality? Anyone working on it? Plus another dose of unintended consequences. A brief episode with Health Hats.
Blog subscribers: Listen to the podcast here. Scroll down through show notes to read the post.
Subscribe to Health Hats, the Podcast, on your favorite podcast player
Episode Notes
Prefer to read, experience impaired hearing or deafness?
Find FULL TRANSCRIPT at the end of the other show notes or download the printable transcript here
Contents with Time-Stamped Headings
to listen where you want to listen or read where you want to read (heading. time on podcast xx:xx. page # on the transcript)
National collaboratives 03:47. 2
Please comments and ask questions
- at the comment section at the bottom of the show notes
- on LinkedIn
- via email
- DM on Instagram or Twitter to @healthhats
Credits
Music by permission from Joey van Leeuwen, Boston Drummer, Composer, Arranger
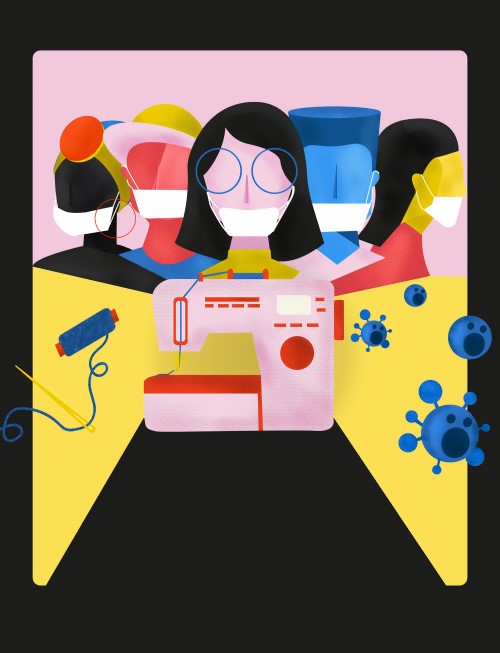
Photo by United Nation COVID-19 Response on Unsplash
Photo by Sandie Clarke on Unsplash
Thanks to these fine people who inspired me for this episode: Ann Boland, Laura Marcial, Michael Waters, Michael Mittelman, Brian Alper, Joyce Lee, Maria Michaels
Links
National COVID Cohort Collaborative (N3C) at the NIH collecting data from electronic health records
PCORI (Patient-Centered Research Institute)-sponsored HERO Registry for healthcare worker exposure
The Covid-19 Knowledge Accelerator with systematic reviews of research
Private industry’s COVID-19 Healthcare Coalition
Datavant’s COVID-19 Research Database
Mothers Out Front environmental justice
Individualized risk predictor.
Yale personal risk calculator, Hunala.
Washington Post article, Climate change is also a racial justice problem
Related podcasts and blogs
About the Show
Welcome to Health Hats, learning on the journey toward best health. I am Danny van Leeuwen, a two-legged, old, cisgender, white man with privilege, living in a food oasis, who can afford many hats and knows a little about a lot of healthcare and a lot about very little. Most people wear hats one at a time, but I wear them all at once. We will listen and learn about what it takes to adjust to life’s realities in the awesome circus of healthcare. Let’s make some sense of all this.
To subscribe go to https://health-hats.com/
Creative Commons Licensing
The material found on this website created by me is Open Source and licensed under Creative Commons Attribution. Anyone may use the material (written, audio, or video) freely at no charge. Please cite the source as: ‘From Danny van Leeuwen, Health Hats. (including the link to my website). I welcome edits and improvements. Please let me know. danny@health-hats.com. The material on this site created by others is theirs and use follows their guidelines.
The Show
Calculating risk
This morning my wife, an outpatient occupational therapist in a satellite clinic, asked, ‘Is it safe for me to still go to work? Is it worth the risk? Everyone wears a mask; we mostly stay six feet apart; the room is well ventilated with the air drawn up.’ She drives to work. I’m over 65, male, with multiple sclerosis on immunosuppressant infusions.
I want to go to the literature and find a risk calculator that produces a score given the factors of age, gender, home and work zip code, the density of work, transportation method, pre-existing conditions, and job risk. And combine that with local stats for COVID positive rates, mortality, mask-wearing/social distancing use, testing percentages. Enter the data, and the calculator would say my wife has a certain range of risk, perhaps a 1-5% chance of contracting COVID-19, and if she gets it a 0.5 – 6% chance of dying of it (numbers made up, of course) and the same for me.
$64 billion question
‘Don’t be silly’, you say, ‘we don’t have the data for that.’ I respond, why not? Aren’t those the $64 billion questions everyone asks? Is anyone funding the research so the risk could be calculated? What’s AI (Artificial Intelligence) for anyway? Every conversation at work, home, or in the real or virtual street includes some variation of risk assessment. Should my kid or I go to work or school today, next month? Should I go to the hospital in an emergency? Can the family get together for Thanksgiving? We should be able to plug our personal information into a web form and get a risk percentage. Hematologists can tell us the risk of mortality for various cancer treatments. You say, ‘data about populations don’t say anything about the individual.’ But isn’t that what research does –inform individuals about the likelihood of some outcome, like mortality, recovery, unintended consequences, based on an understanding of groups of people in specific settings?
National collaboratives
 I accept we aren’t there yet. But are we moving in that direction? I don’t know. We don’t have a concerted nationwide effort to know. I am aware of many COVID collaborations funded and unfunded. National COVID Cohort Collaborative (N3C) at the NIH collecting data from electronic health records; PCORI (Patient-Centered Research Institute)-sponsored HERO Registry for healthcare worker exposure; the Covid-19 Knowledge Accelerator with systematic reviews of research; private industry’s COVID-19 Healthcare Coalition; and Datavant’s COVID-19 Research Database come to mind plus many, many, many more. I haven’t yet found a funded collaborative that answers the questions we as community members ask to manage our lives safely. Perhaps our data isn’t helping us make decisions because we don’t have the right data. Without national leadership and public-private partnership, this will move slowly. People need answers now. See links in the show notes for all the resources mentioned here.
I accept we aren’t there yet. But are we moving in that direction? I don’t know. We don’t have a concerted nationwide effort to know. I am aware of many COVID collaborations funded and unfunded. National COVID Cohort Collaborative (N3C) at the NIH collecting data from electronic health records; PCORI (Patient-Centered Research Institute)-sponsored HERO Registry for healthcare worker exposure; the Covid-19 Knowledge Accelerator with systematic reviews of research; private industry’s COVID-19 Healthcare Coalition; and Datavant’s COVID-19 Research Database come to mind plus many, many, many more. I haven’t yet found a funded collaborative that answers the questions we as community members ask to manage our lives safely. Perhaps our data isn’t helping us make decisions because we don’t have the right data. Without national leadership and public-private partnership, this will move slowly. People need answers now. See links in the show notes for all the resources mentioned here.
Now a word about our sponsor, ABRIDGE.
Use Abridge to record your doctor visit. Push the big pink button and record the conversation. Read the transcript or listen to clips when you get home. Check out the app at abridge.com or download it on the Apple App Store or Google Play Store. Record your health care conversations. Let me know how it went!”
Evidence-informed guidance – where are you?
I am working on part of this with a small band of volunteers. We’re trying to picture and formulate the problem, suggest an approach, and find people with passion and means to carry it forward. So far, we see the problem as: How can the research industry help laypeople and communities find evidence-informed guidance to live safely? Guidance that answers their questions, when needed, in a familiar manner, that they trust? We are exploring what patient-centered means in these circumstances? How can we be inclusive of the awesome diversity of our communities? How can laypeople find what they need, when they need it, in a manner that’s useful? What about our epidemic of mistrust in science and evidence? More to come. Let me know your thoughts. Comment here or email mailto:tech.safeliving@gmail.com
Unintended Consequences
 During my last short, on-mic episode, Unintended Consequences, I promised to offer regular examples of unintended consequences as I observe them. This one occurred to me while hearing my wife talk about an initiative, Mothers Out Front. Climate change initiatives can have a temporary or sustained unequal impact on communities. I live in an upper-middle-class community with increasing numbers of homes with solar panels, a town-sponsored drive to push the all-renewable electricity option from our supplier, my grandson counts Teslas. We have a Chevy Bolt. As our hoped-for success unfolds, those who can’t afford the increased cost of renewable-source electricity, solar panels, or solar cars continue to use now less expensive oil and natural gas. As fewer people and industries use non-renewable energy, the high, sunk, infrastructure costs remain. Those with fewer means will pay more in their utility bills until equity policy catches up with infrastructure changes. Indeed, a strong case exists for environmental justice. The case is robust and broad, including the unequal cost on more impoverished communities of pollution, accidents, and disasters as discussed in the Washington Post article, Climate change is also a racial justice problem. As we consider righteous policy and practice change, do we also address some populations’ potential unfavorable impact? Unintended consequences.
During my last short, on-mic episode, Unintended Consequences, I promised to offer regular examples of unintended consequences as I observe them. This one occurred to me while hearing my wife talk about an initiative, Mothers Out Front. Climate change initiatives can have a temporary or sustained unequal impact on communities. I live in an upper-middle-class community with increasing numbers of homes with solar panels, a town-sponsored drive to push the all-renewable electricity option from our supplier, my grandson counts Teslas. We have a Chevy Bolt. As our hoped-for success unfolds, those who can’t afford the increased cost of renewable-source electricity, solar panels, or solar cars continue to use now less expensive oil and natural gas. As fewer people and industries use non-renewable energy, the high, sunk, infrastructure costs remain. Those with fewer means will pay more in their utility bills until equity policy catches up with infrastructure changes. Indeed, a strong case exists for environmental justice. The case is robust and broad, including the unequal cost on more impoverished communities of pollution, accidents, and disasters as discussed in the Washington Post article, Climate change is also a racial justice problem. As we consider righteous policy and practice change, do we also address some populations’ potential unfavorable impact? Unintended consequences.
Thanks, folks. Onward.

Hi Danny, Yes to your musings. This is an important questions to me: calculating Covid risk.
I just downloaded an ap to my computer on Friday–saw it on a FB post from a Delmar Doctor, https://mycovidrisk.app/
I wanted to calculate the risk of having a couple friends sit with me in my disinfected living room, masked, at least 6 feet distant, windows open) on a cold rainy day. We’ve been sitting in a backyard lots of the summer, masked distant–but the weather’s changing. I think we need to get plastic face shields on top of our masks to lower our medium low risk even further. I also had a fan blowing out in one of the open windows–and the app did not have that as a variable. I was pretty nervewracked about doing this–but the friend is 87 years old and vulnerable, and also need very much to connect with good friends since she’s mostly shut in, and will be in the winter even more so.