Understanding someone else's experience - oh my, so hard! It's difficult enough to understand my…
DannyAugust 17, 2014
A car rental experience from hell. Took 2 1/2 hours to complete car rental. Poor…
DannyJune 22, 2014
This week I heard someone speak about the importance for everyone to have the opportunity…
DannyJune 8, 2014
Sudden, severe illness or protracted undefined illness likely causes a family health crisis. Families in…
DannyJune 1, 2014
Worry, a familiar and unwelcome companion on the health journey. What do I have? Will…
DannyApril 20, 2014

Yesterday I played in a recital with my jazz combo-dedicated amateurs. Musically we have greatly…
DannyApril 13, 2014
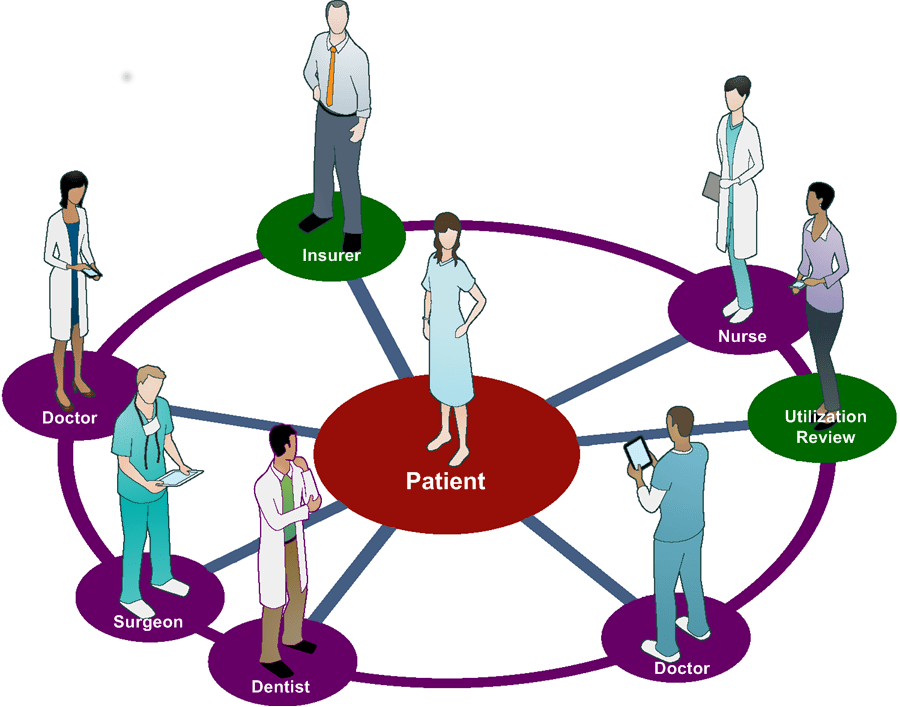
Much of health care depends on relationships. What do people at the center of care…
DannyMarch 16, 2014